Developments in Drug Delivery Featured Signal of Change: SoC806 June 2015
SoC770 — Implantable Health-Care Devices and SoC762 — Health-Care Devices to Stick On look at new developments in wearable diagnostic devices and treatment technologies in health-care applications. Drug-delivery technology is experiencing a similar period of rapid development, and research institutions are working on novel ways to ensure that medication releases more effectively and, in many cases, directly targets the organs that require the pharmaceuticals. Currently, patients can easily forget to take their medication, and many do. Patients' compliance with and continued adherence to prescribed medication regimens—which include dosage, dosing schedule, and treatment duration—are critical not only to treating medical conditions successfully but also to keeping health-care costs under control. In the United States alone, noncompliance with prescribed medication regimens costs between $100 billion and $289 billion annually.
Many technologies release medication over time in very controlled ways, and some activate a drug only when the patient requires medication.
Novel drug-delivery technologies offer a wide range of benefits. Many of these technologies release medication over time in very controlled ways, and some activate a drug only when the patient requires the medication. Other technologies enable the treatment of the affected organ without flooding the entire body with pharmaceuticals. Some novel types of drug delivery require only slight adjustments to existing practices and technologies, whereas others are revolutionary—for example, some researchers envision nanoparticle swarms that detect and fight diseases. Novel approaches to highly controlled drug delivery are proliferating. Indeed, a new field is emerging around the use of advanced technologies to simplify and increase the efficacy of drug delivery. To commercialize new drug-delivery applications, researchers will have to identify the potential dangers of new practices and ensure that materials in use are nontoxic. In addition, such applications will require legislative approval from various government institutions. New drug-delivery applications that do make it to the market could prove tremendously beneficial—for instance, proper use of vaccines, medications, and treatments has a massive impact on health-care costs and patient outcomes.
Advances in drug delivery will enable medical staff to prescribe medication regimens that patients can adhere to with minimal discipline. For instance, researchers at the Massachusetts Institute of Technology (MIT; Cambridge, Massachusetts) developed a modified insulin that could simplify diabetes treatment. During testing in mice, the insulin responded quickly to fluctuations in blood-sugar levels and remained circulating in the bloodstream for a minimum of ten hours. And researchers at Baylor College of Medicine (Houston, Texas) developed polymer nanowafers that are about one-tenth the size of contact lenses and store drugs in an array of very small reservoirs. The nanowafers, which users wear like contact lenses, release medication gradually throughout the day and could replace medicinal eyedrops. Perhaps offering a glimpse of what medication might look like in the future, scientists at the Wyss Institute for Biologically Inspired Engineering at Harvard University and the Harvard School of Engineering and Applied Sciences (both Harvard University; Cambridge, Massachusetts) "show a non–surgical injection of programmable biomaterial that spontaneously assembles in vivo into a 3D structure could fight and even help prevent cancer and also infectious disease such as HIV" ("Injectable 3D vaccines could fight cancer and infectious diseases," Wyss Institute for Biologically Inspired Engineering at Harvard University, 8 December 2014; online). The biomaterial, which doctors administer via a minimally invasive subcutaneous injection, comprises mesoporous silica rods that carry drug components in nanopores.
Injectable and implantable materials that store medication and release it over time likely will become common in the future, offering patients unprecedented convenience. Chemical engineers at MIT have developed an injectable hydrogel that can carry drugs for treating a number of diseases. The gel is a mesh of "nanoparticles made of polymers entwined within strands of another polymer, such as cellulose" ("New nanogel for drug delivery," MIT News Office, 19 February 2015; online). Following its injection, the gel stays in place to deliver drugs to a specific region over time. Because the gel features two components, it could deliver two kinds of drugs simultaneously. At present, treatment options for osteoarthritis are limited, but researchers at Queen Mary University of London (London, England) have developed a treatment to reduce the inflammation that can occur in cartilage that has been affected by the incurable, degenerative disease. Studies have shown that the protein molecule C-type natriuretic peptide (CNP) can reduce inflammation and even reverse tissue damage; however, CNP breaks down very easily, which prevents it from reaching and treating the targeted site after injection. To overcome this problem, the researchers created injectable 2-micron-diameter microcapsules that carry CNP to a target site and then slowly release the CNP to treat the damaged area.
More advanced and experimental drug-delivery and treatment approaches are also under development. For example, during tests on mice, researchers from Brigham and Women's Hospital (Boston, Massachusetts) and Columbia University Medical Center (New York, New York) used targeted nanoparticles to deliver molecules of an anti-inflammatory drug to arterial fat deposits. The drug molecules were able to restructure mice's atherosclerotic plaques, making them more stable. The researchers predict that this approach would have a similar effect in humans and may be able to prevent heart attacks and strokes resulting from atherosclerosis. And Sabine Hauert from the Bristol Robotics Laboratory (Bristol, England) wants to give nanoparticles swarm intelligence to enable medical applications. Because nanoparticles are too small to contain electronics and cannot run software, programming them represents a major hurdle. Dr. Hauert has worked with MIT's Sangeeta Bhatia—a pioneer in the use of miniaturized biomedical tools to attack cancer—and believes that a nanoparticle's coating, electrical charge, shape, size, and material can have an effect on the nanoparticle's functionalities. Nanoparticle design could therefore represent a type of programming. To find promising nanoparticle designs, Dr. Hauert leveraged NanoDoc—"an online game that allows bioengineers and the general public to design new nanoparticle strategies towards the treatment of cancer" (http://nanodoc.org). Researchers at MIT's Laboratory for Multiscale Regenerative Technologies designed the game, which launched in 2013. The game crowdsources nanoparticle designs and simulates the behavior of the nanoparticles that players create.
The Development of this Signal of Change
Data Points
- SC-2015-05-06-081
Researchers at Baylor College of Medicine have developed small polymer nanowafers that can store drugs in an array of very small reservoirs. - SC-2015-05-06-013
Chemical engineers at MIT have developed an injectable hydrogel that can carry drugs for treating a number of diseases. - SC-2015-05-06-003
Researchers at Queen Mary University of London have created microcapsules that can slowly release protein molecules into the body.
Implications
Developments in Drug Delivery
Novel drug-delivery technologies offer a wide range of benefits.
Previous Alerts
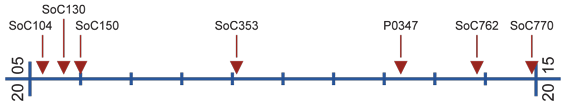
- SoC104 — When Form Is Function (April 2005)
For many phenomena in nature, form relates so closely to function that the two traits are indistinguishable. - SoC130 — Nanomedicine (September 2005)
Researchers are intent on devising medical interventions that either cure disease or treat damaged and diseased tissue at the level of both single molecules and molecular assemblies. - SoC150 — Toward Customized Medicine (January 2006)
As scientists continue their pursuit of customized medicine through research in molecular biology and genetics, the broader social community is beginning to recognize and address infrastructure, regulatory, and policy needs and issues. - SoC353 — Pills for Every Purpose (February 2009)
Reaching beyond traditional medicinal or nutritional purposes, researchers are inventing pills to help consumers with a variety of life's problems. - P0347 — Fantastic Voyage: Robots in the Body (May 2012)
Researchers are considering new types of devices that they can embed or release in the body of a patient to deliver medical treatment. Some of the devices are simple and wireless, and others are fairly sophisticated diagnostics tools. - SoC762 — Health-Care Devices to Stick On (November 2014)
Efforts to develop stick-on health-care devices are manifold. Effective combination of sensors, power provision, and transmission and storage of data are issues developers have to deal with. - SoC770 — Implantable Health-Care Devices (December 2014)
Implantable sensors that enable continuous, uninterrupted monitoring of data likely will play a more important role in the future.